I would say I have always suffered from a weakness in my lower back. Years of sports, a couple of car accidents and lifting incorrectly, just say I learnt the hard way. After a couple of bouts of frustrating acute back pain, I now follow what I call a “back management plan”. Basically I never lift anything that looks too heavy and I follow a back supporting exercise regime. So I was taken by surprise when a few weeks ago from nowhere I had excruciating lower back pain.
I am not one for pain killers, my first port of call was a fantastic colleague Caroline Clarke http://www.carolinejclarke.com/ who is an expert in the Egoscue method of Postural Alignment. Following a couple of consultations she diagnosed a tight psoas muscle, and prescribed a bespoke exercise programme to support this prognosis. On the second consultation she began to mention links with a ‘tight’ psoas and gut complaints. Obviously as a Nutritional Therapist this was a light bulb moment, as I also has had a number of gut symptoms. This led me to wanting to know more about this important muscle, and how supporting could also include a need for a gut protocol.
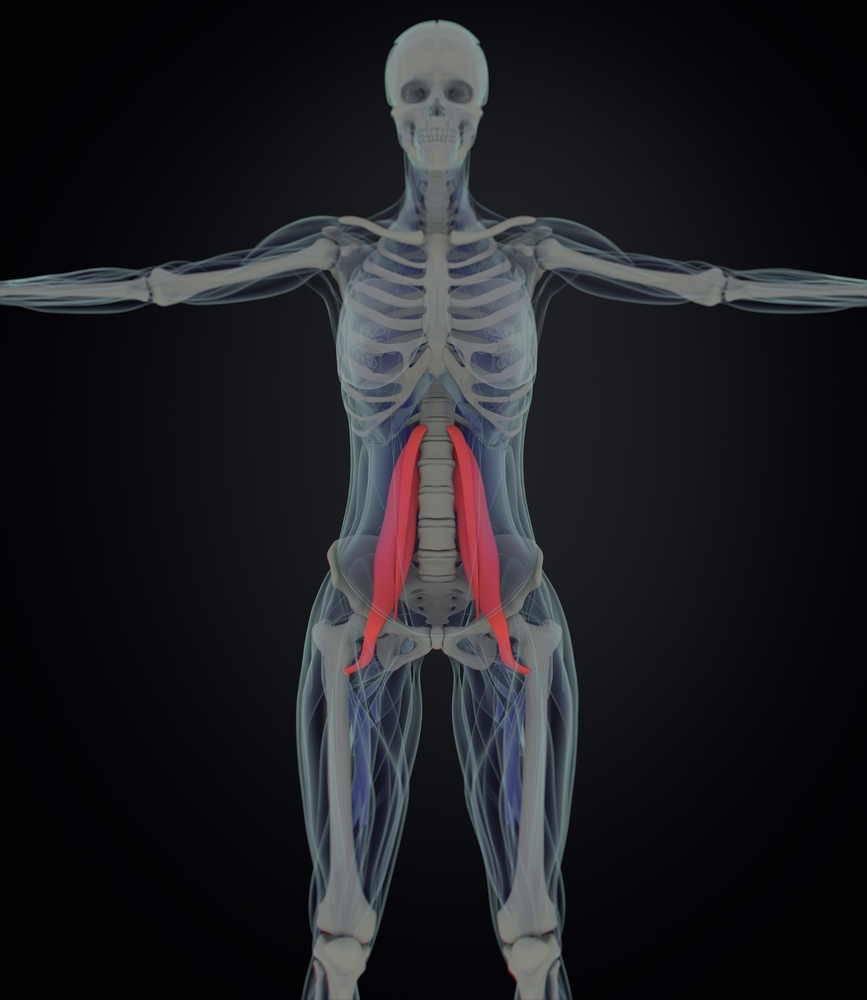
The Psoas Explained:
The psoas is the body’s most important muscle for a number of reasons—it is the walking muscle as each successful step is initiated by the psoas major; along with the piriformis muscle it helps our spine stay upright (they, along with the gluteus maximus are the only three muscles that connect the legs to the spine).
Two muscles, the psoas major and the illacus, together make up what is known as the illiopsoas complex or simply, the psoas. This muscle group is one of the most important in the entire body. Because of its location, it is one of the major muscles that allows us to stand upright, connecting our spine to our legs from the front. The psoas begins at the long head of the femur (thigh) bone and wraps up over the front of the pelvis. The illiacus then attaches to the inside of the pelvis, while the psoas major draws back and connects to the sides of our lumbar vertebrae. Functionally, this is the muscle that pulls our knees towards our chest. It is also one of the main core muscles involved in the body’s “fight, flight or foetal” response.
Tight Psoas / Psoas Syndrome
Being me I began to question what is a tight Psoas muscle and why would it have an impact on my gut? First I hypothesised that the muscle could apply pressure across the lower abdomen but also prolonged ongoing stress (fight or flight) triggered by pain could also have an impact on the gut and lead to an imbalance in the digestion or dysbiosis.
From the literature I read I found a tight psoas muscle can also be called Psoas Syndrome which will typically present as a lower back abdominal/pelvic pain, and may radiate to the leg as the branches of the lumbar plexus pass through the muscle. Pain may worsen by hip flexion, passively or against resistance, as well as during extension of the hip joint.
The psoas muscle is deep to the appendix, and therefore may be irritated with appendicitis. It also may present as a deep abdominal pain.
Before the lower back pain started I had symptoms of a rumbling appendix, an uncomfortable feeling in my gut with bloating and lower abdominal pain. The literature also confirmed that a tight psoas muscle stretch’s over the lower abdomen causing pressure on that area which can result in bloating and abdominal pain.
Psoas and the link with the Stress Response: Fight or Flight
Not only does your psoas muscle intiate bending from the hip and stabilize your trunk and spine during movement and sitting. It also support your internal organs and work like hydraulic pumps allowing blood and lymph to be pushed in and out of your cells.
Your psoas muscles are vital not only to your structural well-being, but also to your psychological well-being because of their connection to your breath.
Here’s why: There are two tendons for the diaphragm (called the crura) that extend down and connect to the spine alongside where the psoas muscles attach. One of the ligaments (the medial arcuate) wraps around the top of each psoas. Also, the diaphragm and the psoas muscles are connected through fascia that also connects the other hip muscles.
These connections between the psoas muscle and the diaphragm literally connect your ability to walk and breathe, and also how you respond to fear and excitement. That’s because, when you are startled or under stress, your psoas contracts.
In other words, your psoas has a direct influence on your fight or flight response!
During prolonged periods of stress, your psoas is constantly contracted. The same contraction occurs when you:
- sit for long periods of time
- engage in excessive running or walking
- sleep in the foetal position
- do a lot of sit-ups
All of these activities compress the front of your hip and shorten your psoas muscle.
Supporting the Stress Response with Nutrition
As a Nutritional therapist the link between prolonged stresses such as that caused by Psoas Syndrome can lead to a number of gastro-intestinal symptoms. The gastrointestinal tract and the immune system are particularly responsive to different stressors. Stress may affect different physiologic functions of the gastrointestinal tract including gastric secretion, gut motility, mucosal permeability and barrier function, visceral sensitivity and mucosal blood flow. In recent years the important interplay between stress and gut microbiota has been shown. The central nervous system and the gut are intimately connected so you can start to see the link between stress and gastrointestinal diseases. During the fight or flight response are digestion ‘shuts down’. It is well known that exposure to stress may lead to the manifestation of different symptoms within the gastrointestinal tract such as bloating, constipation, diarrhoea or abdominal pain.
If a person presents in clinic with pain and gut symptoms the 5R programme is a tried and tested method to regain gut health alongside recommended exercise by a qualified health professional.
An easy way to take those steps to a healthy gut microbiome is to follow a very successful protocol called the 5Rs, which stands for Remove, Replace, Reinoculate, Repair and Retain.
The programme simplifies the complex interactions and systems by following five main steps:
Remove support stresses in your life such as pain but also you may find that certain foods that may cause symptoms such as bloating, constipation even itchy skin conditions such as eczema try to eliminate. If you find your symptoms get worse after eating a type of food try and remove it for 4 weeks or just have a rest from processed and refined and sugary foods such as cakes, pastries and packaged savoury items.
Replace the replenishment of enzymes and other digestive factors lacking or in limited supply in an individual’s GI environment. First think about how you eat if needed try to slow down whilst eating and don’t eat on the run, sit at a table. By slowing down you allow your body time to activate the enzymes you need to start the digestive process. Chewing your food properly also aids in the breaking down of food and finally sitting down at a table or just stopping is a calmer and less stressful way to eat your food. You may need to consider taking a digestive enzyme supplement for a few weeks.
Reinoculate refers to the reintroduction of desirable bacteria, or pre and probiotics, into the intestine to re-establish microflora balance.
Repair involves providing nutrients which will facilitate complete repair of the damaged gut. Glutamine is the most abundant amino acid (protein building block) in the body and is involved in more metabolic processes than any other amino acid. Glutamine is the preferred fuel of the cells that line the small intestine and is therefore vital to the health of the intestine as a whole. You could say it is like a moisturising cream for your insides.
Retain, Retaininga healthy gut function is further facilitated by eating healthily, taking regular exercise, managing stress (pain), ensuring good quality sleep and applying foundation nutritional support, such as fibre, multivitamins and minerals, probiotics and l-glutamine.
If you have any of these symptoms perhaps ask the question from a health care professional do you think it may be my Psoas Muscle?
Psoas pain can manifest in many ways both directly and indirectly through its relationship to surrounding muscles. Pain in the lower back can come from a tight psoas that has compressed the lumber spine.
- Pain in the hip socket can be the result of a tight psoas pulling the head of the femur too deeply into the socket of the acetabulum.
- There is often a wrapping pain associated with the psoas that starts at the back of the inner thigh wrapping up and around to the rim of the pelvis. I believe this is from the tight psoas putting pressure on the inguinal ligament that helps strap the psoas down.
- Pain in the outer hip or IT band can be the result of a tight psoas externally rotating the leg and putting undo pressure on the outer thigh.
- If one or both of the psoas are tight they can cause abdominal cramping or bloating
- In addition to this lovely list of ailments, dysfunction in the psoas can also be related foot pain, knee pain, shoulder pain etc.
Since many experts don’t understand the complexity of the psoas muscles, it’s not uncommon for people to be given the wrong diagnoses and treatments for their psoas-related pain.
Thank you for reading. Please see my facebook page @finutrition for more information on events etc..
Please do not make any changes to how you eat or take food supplements without consulting a healthcare professional, especially if taking medication.