Coeliac disease is a serious illness where the body’s immune system attacks its own tissues when you eat gluten. This causes damage to the lining of the gut and means the body can’t properly absorb nutrients from food. Coeliac disease is not an allergy or food intolerance.
Gluten is a protein found in wheat, and other similar proteins found in rye, barley and oats. These proteins damage the small finger-like projections (villi) that line the small intestine, resembling a pile in a carpet, and play a significant role in digestion (Fig.1). When damaged and inflamed, the villi are unable to absorb water and nutrients such as vitamins, folic acid, iron and calcium. This causes the coeliac to be susceptible to a variety of other conditions related to malabsorption, including lactose intolerance.
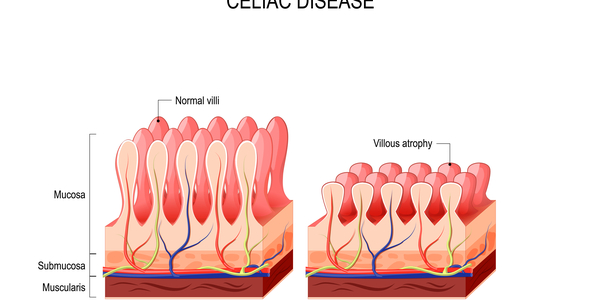
Fig 1: Healthy and damaged villi
Apart from the inability to absorb nutrients, damaged lining to the small intestine has other negative results. It is unable to produce sufficient digestive enzymes essential to break down foods for complete digestion and absorption, such as lactose and carbohydrates. Large components of foods remain in the digestive tracts unabsorbed which are in turn fermented by bacteria living naturally in our digestive tract and ideal conditions causing cramps, gas, bloating, flatulence and diarrhoea.
Once diagnosed, the only treatment for coeliac disease is a gluten free diet. Gluten is found in wheat, barley and rye. Some people are also sensitive to oats. Once gluten is removed from the diet, you should start to feel much better.
Gluten is composed of gliadins and glutenin’s, only the gliadin portion triggers Coeliac disease. Rice for example, contains glutenin’s and can therefore be tolerated. In rye, barley and oats, the proteins that activate the disease are termed secalins, hordeins and avenins.
You should also take care and read food labels for hidden sources of gluten such as: Hydrolysed plant / vegetable protein, all derivatives if wheat, rye, oats and barley, malt, modified food starch, soy sauce, vinegars, binders, fillers, ‘natural flavourings’, non-dairy creamers, curry powders and seasonings.
Coeliac disease is common and affects one in 100 people. However only 30% who have the condition have been diagnosed which means there are currently nearly half a million people who have coeliac disease but don’t yet know. If a first degree family member (such as mother, father, sister or brother) has the condition then the chances of having it increase to one in ten.
Dermatitis herpetiformis (DH) is the skin manifestation of coeliac disease which occurs as a rash that commonly occurs on the elbows, knees, shoulders, buttocks and face, with red, raised patches often with blisters. It affects around one in 3,300 people.
A few Myths
Coeliac disease is a food allergy’…myth
Coeliac disease is not a food allergy or an intolerance, it is an autoimmune disease. In coeliac disease, eating gluten causes the lining of the small intestine to become damaged. Other parts of the body may be affected.
‘You have to have gut symptoms such as diarrhoea to have coeliac disease’…myth
Coeliac disease is known as a ‘multi-system’ disorder – symptoms can affect any area of the body. Symptoms differ between individuals in terms of type and severity.
Coeliac disease can develop and be diagnosed at any age. It may develop after weaning onto cereals that contain gluten, in old age or any time in between. Coeliac disease is most frequently diagnosed in people aged 40-60 years old. Delayed diagnosis is common, and research shows the average time it takes to be diagnosed is 13 years.
Recent research suggests that most people with coeliac disease are of normal weight or overweight at diagnosis. Body weight alone should not be used to decide whether or not you should be tested for coeliac disease.
Coeliac disease is a lifelong condition. The gluten-free diet is the only treatment for coeliac disease. If gluten is introduced back into the diet at a later date, the immune system will react, and the gut lining will become damaged again. If someone following a gluten-free diet is retested for coeliac disease (antibody blood test, gut biopsy) it would be expected that the tests are negative. This means they are responding well to the gluten-free diet. There are no antibodies in the blood because there is no gluten for the immune system to react against. Taking gluten out of the diet allows the gut to heal.
‘A breadcrumb won’t hurt someone with coeliac disease’…myth.
Even very small amounts of gluten can be damaging to people with coeliac disease. Therefore, taking sensible steps to avoid cross contamination with gluten is important.
Top tips include:
- keep cooking utensils separate during food preparation and cooking
- avoid frying food in the same oil that has previously been used to cook foods which contain gluten
- use a clean grill, separate toaster or toaster bags to make gluten-free toast
- use separate breadboards and wash surfaces thoroughly
- use separate condiments like jam, butter, mustard and mayonnaise.
Diagnosis
There are specific blood tests used to diagnose coeliac disease. They look for antibodies that the body makes in response to eating gluten. Your GP will carry out a simple blood test to check for these antibodies.
In adults, with suspected coeliac disease, the following blood tests are recommended:
- Total immunoglobulin A (IgA)
- IgA Tissue transglutaminase antibody (shortened to tTG)
If IgA tTG is weakly positive, then IgA endomysial antibodies (shortened to EMA) should be used.
In children with suspected coeliac disease, the following blood tests are recommended:
- Total IgA
- IgA tTG
It’s important to continue eating gluten until you have had a blood test and gut biopsy. If you remove or reduce the amount of gluten in your diet before testing this will affect your result. Guidelines recommend that you eat some gluten in more than one meal every day for at least six weeks before testing.
Negative blood test results
It’s possible to have a negative blood test and still have coeliac disease. If you weren’t eating gluten at the time of your blood test, you may have received an inaccurate result.
If you have ongoing symptoms that suggest coeliac disease but have had a negative blood test, ask your GP to check to see if you have been tested for IgA deficiency.
IgA deficiency
Some people with coeliac disease do not make the usual coeliac disease antibodies. This is called IgA deficiency. When the laboratory is measuring your antibody level, they should also check your total serum IgA to detect IgA deficiency. If you are IgA deficient the following tests should be considered:
- Immunoglobulin G (IgG) EMA
- IgG deamidated gliadin peptide (DGP)
- IgG tTG
If you have a positive blood test for coeliac disease, your GP will refer you to a gut specialist – a gastroenterologist – for a biopsy of the gut. This confirms whether or not you have coeliac disease.
A biopsy involves a small camera called an endoscope being passed through your mouth and stomach into the gut. It is done using an anaesthetic spray to numb your throat, or with a sedative given by injection.
Biopsies are collected and examined under a microscope to check for damage to the gut lining, which is typical of coeliac disease.
The gluten free diet
- If you have coeliac disease and/or dermatitis herpetiformis you have to avoid gluten for life.
- The gluten free diet is the only treatment for the condition.
- On the gluten free diet, you can eat many foods including meat, fish, fruit, vegetables, rice and potatoes.
- You can also eat gluten free substitute foods and processed foods that don’t contain gluten.
- Under new Food Legislation pre-packed food should highlight allergens in the ingredient label
Feeling better
After diagnosis of coeliac disease, healing and how long it takes to feel better on a gluten free diet can vary.
Some people feel significantly better within a few days of cutting out gluten, but some people may see more of a gradual improvement in their symptoms or that one symptom improves before another.
It can take between six months and up to five years (in some cases longer) for the gut damage caused by eating gluten to fully heal. Several factors are thought to be involved in the variable time taken for the gut to heal, including age and severity of gut damage at diagnosis.
If you make a mistake
Following a gluten free diet is a learning process, not only for you but also for your family and friends. Mistakes can happen whilst you’re following a gluten free diet, especially if you have only recently been diagnosed.
If you have coeliac disease and eat gluten by mistake, you would usually start to have symptoms a few hours after eating it and the symptoms can last from a few hours to several days. However, the effects vary from person to person, and depend on how much gluten you’ve eaten, how sensitive you are and how long you have been on a gluten free diet.
Working with a health care professional such as a Nutritional Therapist can help guide and support you in making the correct food choices. Just removing gluten containing foods may leave a huge gap in your daily food intake. Suitable alternatives are essential, not only to support your diagnosis but also support the healing of your gut and addressing any underlying nutritional deficiencies.
What is the Connection between Coeliac Disease and Thyroid Disease?
- A significant number of patients with thyroid disease also have coeliac disease
- People with autoimmune thyroid disease are at a higher risk than the general population of having coeliac disease. Between 1.5% – 3.8% of people with autoimmune thyroid disease also have coeliac disease compared to 1% in the general population.
- Symptoms of undiagnosed coeliac disease may be different in patients who also have thyroid disease. Recent studies show it may be beneficial to screen those with thyroid disease for coeliac disease as well.
- At this time, research does not support the use of gluten-free diets in the routine treatment of thyroid disease. While it is not clear whether a gluten-free diet can help in the treatment of thyroid disease alone, it is important to remain on a strict gluten-free diet if you have also been diagnosed with coeliac disease
- It has been postulated that when the immune system attacks gliadin, the antibodies also attack the thyroid. As the immune response continues, the thyroid suffers damage for up to 6 months after gluten consumption.
Thank you for reading my article any questions please see contact page.
