Thank you to all for listening in to the talk on Antibiotics. As promised here is the summary. Next Tuesdays I will be having a break but back the following week with a Nutrition Talk on the topic Parkinson’s`
‘Antibiotics are used to treat or prevent some types of bacterial infection. They work by killing bacteria or preventing them from spreading. But they do not work for everything. Many mild bacterial infections get better on their own without using antibiotics. Antibiotics do not work for viral infections such as colds and flu, and most coughs and sore throats.
Antibiotics are no longer routinely used to treat:
- chest
infections
- ear infections in children
- sore throats
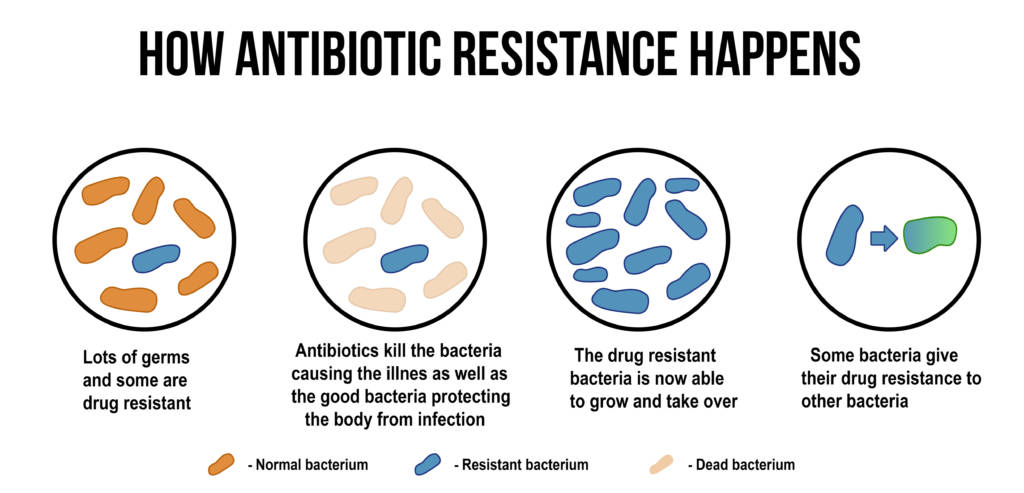
When it comes to antibiotics, take your doctor’s advice on whether you need them or not. Antibiotic resistance is a big problem – taking antibiotics when you do not need them can mean they may not work for you in the future.
When antibiotics are needed
Antibiotics may be used to treat bacterial infections that:
- are unlikely to clear up without antibiotics could infect others
- could take too long to clear without treatment
- carry a risk of more serious complications
- People at a high risk of infection may also be given antibiotics as a precaution, known as antibiotic prophylaxis.
Side effects of antibiotics
common:
- being sick
- feeling sick
- bloating and indigestion
- diarrhoea
- Allergic reaction
- With certain antibiotics or prolonged use, fungal infections of the mouth, digestive tract, and vagina

Less common:
- formation of kidney stones, when taking sulphonamides
- abnormal blood clotting, when taking some cephalosporins
- sensitivity to sunlight, when taking tetracyclines
- blood disorders, when taking trimethoprim
- deafness, when taking erythromycin and the aminoglycosides
Research has shown that antibiotics alter the gut microbiome and host health. Research published on Nature.com has found that thegut microbiome can be permanently perturbed even by short-term or low-dose antibiotic treatment, and that this change can have long-term effects on health.
The microbiome disturbances have the potential to affect the development of several autoimmune, inflammatory and allergic diseases. In another study the results found that children who are exposed to antibiotics in their first year of life had a slightly increased risk of developing asthma, and the risk increased with the number of antibiotic courses. Ongoing research is
Types of Antibiotics
There are hundreds of different types of antibiotics, but most of them can be classified into 6 groups.
Prescription is deponent on what it may be targeting. For example Penicillin’s (such as penicillin and amoxicillin) – widely used to treat a variety of infections, including skin infections, chest infections and urinary tract infections. Whilst Cephalosporins (such as cephalexin) – used to treat a wide range of infections, but some are also effective for treating more serious infections, such as septicaemia and meningitis. Some are only used in hospitals, such as Aminoglycosides to treat very serious illnesses, such as septicaemia, as they can cause serious side effects.
Antibiotic Resistance
Some medical professionals have concerns that people are overusing antibiotics. They also believe that this overuse contributes toward the growing number of bacterial infections that are becoming resistant to antibacterial medications.
Alexander Fleming, speaking in his Nobel Prize acceptance speech in 1945, said:
“Then there is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non-lethal quantities of the drug, make them resistant.”
Why is the Antibiotic Market Broken?
The current economic model for developing new antibiotics is failing. Companies invest huge amounts of money to bring a new drug to market but cannot recover their costs or make a profit. New antibiotics are seen as ‘drugs of last resort’ against dangerous bacteria. So, to limit the development of antibiotic resistance, they need to be used sparingly – and not sold in large volumes. Plus, compared to more expensive treatments, antibiotics tend to be quite low in price. Without financial incentives, many large pharmaceutical companies have started to pull out of the field. In the 1908s there were 18 multinational companies committed to antibiotic research; today there are only a handful.
To counteract the possibility of the risk of antimicrobial resistance (AMR), the NHS will test the world’s first ‘subscription’ style payment model. This model has been developed to incentivise pharmaceutical companies to develop new drugs for resistant infections. The new trial will be led by the National Institute for Health and Care Excellence (NICE) and NHS England and NHS Improvement. It will test a ‘subscription’ style model that pays pharmaceutical companies upfront for access to drugs based on their usefulness to the NHS. This will make it more attractive for companies to invest the estimated £1 billion it costs to develop a new drug, as they can be reassured, they will still be paid for the drug even though it may be stored for reserves. Currently, drugs companies are paid by volume of antibiotics sold, while the NHS is trying to reduce their use to prevent antimicrobial resistance (AMR).
Key Points
- Many mild bacterial infections get better on their own without using antibiotics.
- Antibiotics do not work for viral infections such as colds and flu, and most coughs and sore throats.
- Antibiotic resistance is a big problem – taking antibiotics when you do not need them can mean they will not work for you in the future
- The gut microbiome can be permanently perturbed even by short-term or low-dose antibiotic treatment, and that this change can have long-term effects on health
- The current economic model for developing new antibiotics is failing
Thank you for reading. Please do not start taking supplements without the advice of a trained health professional. My clinic is still running via social media platforms WhatsApp, Skype and Zoom, for more information please email ateatyourgreens@fionawaring.com
Fiona
Waring
Dip Nut,
BSc.(Hons), MSc PHN, ANutr
Nutritional
Therapist
M: +44 07957
267 964
eatyourgreens@fionawaring.com
‘Registered with the Association for Nutrition – www.associationfornutrition.org
Protecting the public and promoting high standards in evidence-based science and professional practice of nutrition.’
