Thank you to all for listening in to the talk on Osteoporosis on Tuesday. As promised here is the summary. Next Tuesdays talk is all about antibiotics.
Osteoporosis is derived from the Latin word, literally means ‘ porous bones’. Osteoporosis weakens bones, making them fragile and more likely to break. It develops slowly over several years and is often only diagnosed when a fall or sudden impact causes a bone to break (fracture).
The most common injuries in people with osteoporosis are:
- broken wrist
- broken hip
- broken spinal bones (vertebrae)
Due to physiological, nutritional and hormonal differences between males and females – more likely in females.
Who’s affected by osteoporosis?
Osteoporosis affects over 3 million people in the UK. More than 500,000 people receive hospital treatment for fragility fractures (bones that break after falling from standing height or less) every year as a result of osteoporosis.
Osteoporosis: Internal Structure of Bone
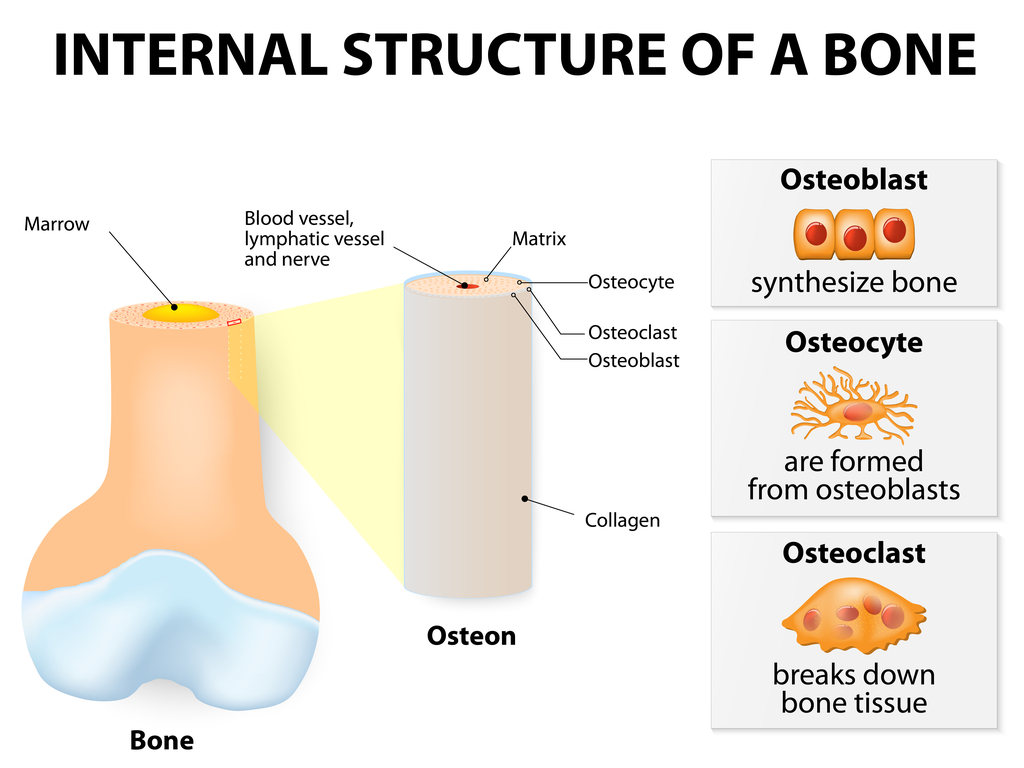
Bone is constantly restoring itself. Cells called osteoblasts make bone, osteoclasts remove old bone as its minerals are absorbed for use elsewhere in the body. If osteoclasts break down the bone quicker than its replaced, bone becomes less dense and therefore likely to break more easily.
Factors that Increase the Risk of Osteoporosis
- taking high-dose steroid tablets for more than 3 months
- other medical conditions – such as inflammatory conditions, hormone-related conditions, or malabsorption problems
- a family history of osteoporosis – particularly a hip fracture in a parent
- long-term use of certain medicines that can affect bone strength or hormone levels, such as anti-oestrogen tablets that many women take after breast cancer
- having or having had an eating disorder such as anorexia or bulimia
- having a low body mass index (BMI)
- heavy drinking and smoking
Bone is strongest at around the age of 30, thereafter declines. If sufficient bone mass not accumulated during formative times in childhood, adolescence and early adulthood, or if you lose it too quickly in later years – increased risk of osteoporosis. Due to this it is iimportant to look after bones early in life, not just after menopause.
Bone loss before osteoporosis (osteopenia)

This is when a bone density scan shows you have lower bone density than the average for your age, but not low enough to be classed as osteoporosis.
Osteoporosis Diagnosis: DEXA SCAN
A bone density scan compares your bone density with the bone density expected for a young healthy adult or a healthy adult of your own age, gender and ethnicity.
The difference is calculated as a standard deviation (SD) score. This measures the difference between your bone density and the expected value. The difference between your measurement and that of a young healthy adult is known as a T score, The difference between your measurement and that of someone of the same age is known as a Z score.
Standard deviation is a measure of variability based on an average or expected value. A T score of:
- above -1 SD is normal
- between -1 and -2.5 SD shows bone loss and is defined as osteopenia
- below -2.5 shows bone loss and is defined as osteoporosis
If your Z score is below -2, your bone density is lower than it should be for someone of your age.
Although BMD results provide a good indication of bone strength, the results of a bone density scan will not necessarily predict whether you’ll get a fracture. This is because other factors, such as age, sex or whether you have previously had a fall, also determine if you’re likely to sustain a fracture.
Osteoporosis and Calcium deficiency
- Not due to Ca deficiency, but how it is absorbed and used by the body is the important factor, not necessarily the amount consumed.
- Important to also have correct balance of Mg, boron, Potassium, Folic Acid, Vitamins C,D,E, and K and protein all important in battling osteoporosis.
- Taking Ca at bedtime, when it is best absorbed and also aids in sleeping.
Treatment: Medication
- Bisphosphonates slow the rate that bone is broken down in your body. This maintains bone density and reduces your risk of a broken bone.
- Selective oestrogen receptor modulators (SERMs) SERMs are medicines that have a similar effect on bone as the hormone oestrogen. They help to maintain bone density and reduce the risk of fracture, particularly of the spine.
- Parathyroid hormone treatments (such as teriparatide) are used to stimulate cells that create new bone. They’re given by injection.
- Calcium and vitamin D supplements
Good Foods to Eat
Eat plenty of foods high in Ca and Vitamin D. Good sources of easy assimilated Ca include broccoli, chestnuts, clams, dandelion greens, most dark green leafy vegetables, flounder, hazelnuts, kale, kelp, molasses, oats, oysters, salmon, sardines (with bones), sea vegetables, sesame seeds, shrimp, tahini and wheat germ. Eggs, garlic and onions all contain sulphur, needed for healthy bones.
Foods/Drinks to Watch Out For!
- Avoid phosphate containing drinks and foods such as soft drinks and alcohol.
- Avoid smoking, sugar and salt. Limit consumption of citrus fruits and tomatoes – these foods inhibit Ca uptake.
- Consume whole grains and Ca foods at different times.
- Whole grains contain a substance that binds with Ca and prevents uptake.
- Yeast is high in phosphorus, which competes with Ca absorption in the body.
Osteoporosis medications & exercise
Thiazide Diuretics increase blood Ca levels so watch with Ca and Vitamin D supplementation – other types of diuretics decrease Ca requirements.
If you’re at risk of developing osteoporosis, you should take steps to help keep your bones healthy. This may include:
- taking regular exercise to keep your bones as strong as possible: lack of exercise can result in loss of Ca – walking best exercise for maintaining bone loss.
- healthy eating – including foods rich in calcium and vitamin D
- taking a daily supplement containing 10 micrograms of vitamin D
- making lifestyle changes – such as giving up smoking and reducing your alcohol consumption
Key Points
- Osteoporosis weakens bones, making them fragile and more likely to break. It develops slowly over several years and is often only diagnosed when a fall or sudden impact causes a bone to break (fracture).
- Possible to have in one area of the skeleton and not another.
- If sufficient bone mass not accumulated during formative times in childhood, adolescence and early adulthood, or if you lose it too quickly in later years – increased risk of osteoporosis. Don’t just focus after menopause.
- Not due to Ca deficiency, but how it is absorbed and used by the body is the important factor – Co-Factors; Food; Type; Time
- make Lifestyle changes to support your bones!
Thank you for reading. Please do not make any changes to the way you eat before consulting a trained health care professional.
Fiona
Waring
Dip Nut, BSc.(Hons), MSc PHN, ANutr
Nutritional
Therapist
M: +44 07957 267 964
eatyourgreens@fionawaring.com
‘Registered
with the Association for Nutrition – www.associationfornutrition.org
Protecting the public and promoting high standards in evidence-based science
and professional practice of nutrition.’